

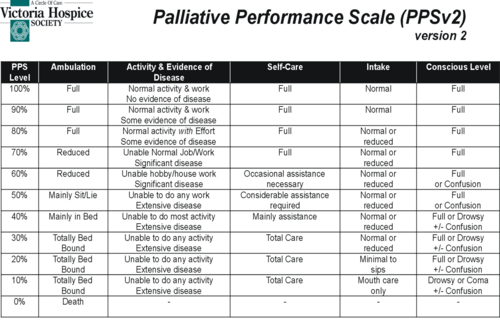
The Palliative Performance Scale

In the PPS[4], physical performance is measured in 10% decremental levels from fully ambulatory and healthy (100%) to death (0%). These levels are further differentiated by five observable parameters:
the degree of ambulation
ability to do activities/extent of disease
ability to do self care
food/fluid intake
level of consciousness
“Stronger” performance indicators are located on the left, and “softer” ones on the right. In determining the patient’s PPS then, we would first find the level that fits with the patient’s ambulation level. From that we would work across the scale keeping in mind that the leftward indicators have more value than those on the right. We can not choose between levels (e.g. 45%). Simply make your best assessment to determine the PPS.
PPS Stages
The PPS can also be broken into three stages:
Stable
Transitional
End-of-Life.
| PPS | Special Concerns |
Stable | 100-70% | - patient/family need for hope/understanding of disease - patient/family education re: disease management, medications, personal care, nutrition, symptom crisis/distress management plan - referrals to optimized functioning - CCAC, physio/OT, dietitian, etc. - psychosocial assessment - spiritual assessment - cultural/religious resources |
Transitional | 60-40% | - most difficult for patients - impacts on all spheres of life (need for holisitic, patient and family-centred care) - requires greatest amount of nursing care - increasing care and educational needs [5] |
End-of-Life | <30% | - review medications/routes of administration, need for further investigations/lab tests/ clinic visits - determine main contact in the community - family physician, homecare, palliative care physician - pain/symptom management - prepare family for death - what do they expect, what are their past experiences with death - ensure affairs are in order - e.g. POA, wills, custody arrangements for children, etc. |
Transitional stage needs:
coordination of care and services
establishment and maintenance of support systems
education of care givers
symptom management
end of life planning[5]
During the Transitional stage, we must consider the psychological, social and economic as well as the physical changes a patient experiences in order to provide holistic, patient and family centred care. Transition is said to be a challenge to a patients’ self-identity. It is therefore, imperative that healthcare professionals have an understanding of the transition process in order to assist patients and their families to move through it. [1]
_________________________________
1. Kralik, D., Visentin, K., & van Loon, A. (2006). Transition: a literature review. Journal of Advanced Nursing, 55(3), 320-329.
3. For more information about the KPS: http://www.acsu.buffalo.edu/~drstall/karnofsky.html http://www.hospicepatients.org/karnofsky.html http://palliative.info/pages/karnofsky.htm
4. Palliative Performance Scale (PPSv2). Medical Care of the Dying, 4th ed.;p.120. copyright Victoria Hospice Society, 2006. http://www.victoriahospice.org/ed_publications.html accessed January 8, 2008
5. Anderson, F., Downing, G.M., Hill, J., Casorso, L., & Lerch, N. (1996). Palliative Performance Scale (PPS): A new tool. Journal of Palliative Care, 12(1), 5-11.
 Previous
Previous