



Communication and Patient Safety
As Director of Patient Safety for Critical Care Medicine at Queen’s University, Dr. Roy Ilan knows that good communication is essential to promoting patient safety.
"There is ample evidence to suggest that ’communication failures’ are a major contributor to adverse events. If we communicate better with each other, the rate of adverse events will decrease dramatically."
Communication is an essential element in patient safety here at Queen’s, around the world and for international bodies such as the World Health Organization.[1]
Breakdown in communication was the leading root cause of sentinel events reported to the Joint Commission in the United States of America between 1995 and 2006
Of the 25 000 to 30 000 preventable adverse events that led to permanent disability in Australia, 11% were due to communication issues, in contrast to 6% due to inadequate skill levels of practitioners.[2]
Is it possible that issues of patient safety may be more related to how we work together than our technical skill or ability to do our work?
These issue are explored in this video produced by the World Health Organization
"...the occurrence of everyday medical mishaps is associated with faulty communication; but poor communication is not simply the result of poor transmission or exchange of information. Communication failures are far more complex and relate to hierarchical differences, concerns with upward influence, conflicting roles and role ambiguity, and interpersonal power and conflict."[3]
"the solutions for improving patient safety offer a more constructive approach - one in which success (safer care) is determined by how well caregivers work together as a team, how effectively they communicate with one another and with patients, and how carefully the care delivery processes and supporting systems of are are designed."[2]
"Open, transparent communication, cooperation and patient involvement are all identified as crucial components in transforming the current system to a safer one."
Use interpreters where needed and available
Write things down even if you have explained them at length
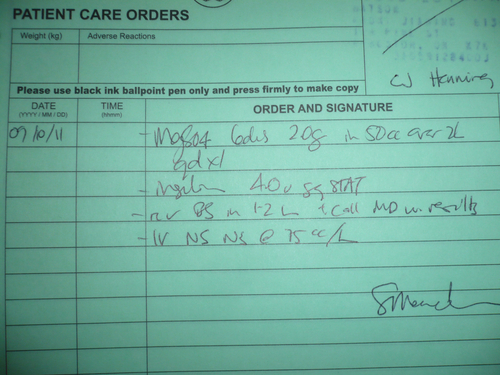
Write legibly, especially when ordering medication!
Ensure people have understood, leave time for questions, ask people what questions they have not if they have questions
Close the loop, make sure everyone has all the information they need and deserve
Forward feed information - give good handover
Face-to-face and person-to-person cannot be replaced, even by the best technology[3]
"Expert communicators are inquisitive, systematic, analytical, open-minded, self-confident, empathetic and receptive. Communication starts to erode in situations in which there is a lack of empathy, respect and trust. It can also be undermined by not actively listening to clients, family members and colleagues." [4]
Written Communication

Write things down for people (medication lists, what to do if there are problems after discharge from hospital, return appointments and follow-up, directions to the lab....)
Write legibly or print things off the computer
Follow the recommendations for safe medication ordering
Read the notes of ALL team members
When writing a consult request, be SPECIFIC with your question
When replying to a consult reply respectfully
Always aim to advance the care of the patient
Writing Orders
One of the major causes of medication errors is the ongoing use of potentially dangerous abbreviations and dose expressions. Underlying factors contributing to many of these errors are illegible or confusing handwriting by clinicians and the failure of health care providers to communicate clearly with one another.[5]
Potentially Dangerous Abbreviations
The Joint Commission has identified common medication errors related to potentially dangerous abbreviations[5]:
DO NOT USE | USE INSTEAD |
U, u (unit) | Write "unit" |
IU (International Unit) | Write "International Unit" |
Q.D., QD, q.d., qd, O.D.,OD (daily) | Write "daily" |
Q.O.D., QOD, q.o.d., qod, E.O.D., EOD, e.o.d., eod, (every other day) | Write "every other day" |
Trailing zero (X.0 mg) | Write X mg |
Lack of leading zero (.X mg) | Write 0.X mg |
MS | Write morphine sulfate |
MSO4, MgSO4 | Write Magnesium sulfate |
AVOID USING | |
< (less than)> (greater than) | Write "less than"Write "greater than" |
Abbreviations for drug names | Write drug names in full |
@ | Write "at" |
cc | Write "mL" (preferred) or "ml" or "millilitre |
The Institute for Safe Medication Practices has a large number of educational resources that can help with the promotion of safe prescribing practices.
You can make your medication orders safer just by USING CAPITAL LETTERS to differentiate look-alike names, instead of cursive or lower case writing.[6] For example: ceFAZolin and cefTRIAXONE.
Handover
"The hand-over (or hand-off) communication between units and between and amongst care teams might not include all the essential information, or information may be misunderstood. These gaps in communication can cause serious breakdowns in the continuity of care, inappropriate treatment, and potential harm to the patient."[2]
Some thoughts and suggestions to improve handover:
"...precise, unambiguous, face-to-face communication was the best way to ensure effective hand-overs."
"...providing opportunities for providers of care to ask and resolve questions can improve the effectiveness of hand-over communications"
"Stream lining and standardizing change-of-shift reporting can enhance critical thinking, as well as minimize time spent away from the patient."
Read-back is a technique where hand-over information is recorded and then the recipient has a chance to read it back to the provider who is handing over to ensure accuracy and completeness
"Collaborative (multi-disciplinary) rounds are being used effectively to improve communication and hand-over of important information relating to the patient’s care."[2]
"Involving patients and families in the process of care is increasingly being recognized as an important aspect of care delivery. The patient and family are the only constant and are thus in a position to play a critical role in ensuring continuity of care. Hospital discharge is a critical stage where communicating information to patients and families becomes vital."[2]
Handover and discharge from hospital are not the only dangerous time for communication. Other communication challenges include:
verbal orders
conflict or past issues with team members
’difficult patient’ label
communicating up the hierarchy
communicating across a power differential
For more information about these and other related topics, please see the Communicating for Patient Safety module.
If you have concerns about patient safety - speak up!
_________________________________
1. The World Health Organization - Patient Safety. Available from: www.who.int/patientsafety/en/ Accessed August 13, 2010
2. World Health Organization. Communication During Patient Hand-overs. Patient Safety Solutions. 2007;May. Available from: www.ccforpatientsafety.org/Patient-Safety-Solutions/ Accessed August 17, 2010
3. Marshall P, Robson R. Preventing and Managing Conflict: Vital Pieces in the Patient Safety Puzzle. Healthcare Quarterly. 2005;8:39-44.
4. Mastering Communication. Angela McNabb RN.p. 2. College of Nurses of Ontario 2006 www.cno.org/pubs/mag/2005/09Sept/feat_comm.htm accessed August 14, 2009
5. The Joint Commission. Sentinel Event Alert. Medication errors related to potentially dangerous abbreviations. Issue 23 - September 1, 2001. Available from: www.jointcommission.org/sentinelevents/sentineleventalert/sea_23.htm
6. Use of TALL MAN LETTERS IS GAINING ACCEPTANCE. ISMP Medication Safety Alert, from July 2008 issue. www.ismp.org/newsletters/acutecare/articles/20080731.asp accesssed September 13, 2010.
 Previous
Previous