



The Duty to Disclose Adverse Events and Report Medical Incompetence
Adverse Events
An adverse events (AE) is:"An event which results in unintended harm to the patient, and is related to the care and/or services provided to the patient rather than to the patient’s underlying medical condition." [5]"unintended injuries or complications resulting in death, disability or prolonged hospital stay that arise from health care management."[1]
Canadian data suggests that in 2000, 1 or more adverse events occurred in 7.5% of acute care hospital admissions, this represents approximately 185 000 admissions. 70 000 of these AEs are potentially preventable.[1]
The Canadian Patient Safety Institute (CPSI) has identified 6 domains of patient safety:
1. Contribute to a culture of patient safety - apply core patient safety knowledge, skills and attitudes to everyday work
2. Work in teams for patient safety
3. Communicate effectively for patient safety
4. Manage safety risks - anticipate, recognize and manage situations that place patients at risk
5. Optimize human and environmental factors
6. Recognize, respond to and disclose adverse events - mitigate harm to patients by ensuring disclosure and preventing recurrence of adverse events and close calls[2] [3]
Harm
Harm has been defined as "an outcome that negatively affects the patient’s health and/or quality of life."[5]
Patient harm may be related to:
inherent risk of procedure - this underlines the importance of informed consent
systemic failures - delay in diagnosis or treatment, or communication problems
provider performance - frank error, lack of skill or training, health or aging issues of provider, one time event vs continuing incompetence
Of course, most often poor outcomes are not the result of ’harm’ but of the failure of the appropriate treatment to be effective.
Medical provider error can be defined as an act (plan, decision, choice, action or inaction) that in retrospect was not correct and resulted in an adverse event or close call. We are all only human and must balance the protection of the public from harm with fairness to providers.
Disclosure of Adverse Events
The CMA Code of Ethics clearly tells us that we must: "Take all reasonable steps to prevent harm to patients; should harm occur, disclose it to the patient."[7]
Physicians and trainees are encouraged to disclose adverse events to the patient, even if no harm has occurred as in the case of a ’close call’ or ’near miss’. Be aware that you may be subject to civil liability for failure to disclose, even if there is no other harm.
The CMPA suggests that they should be contacted whenever there is an adverse event, especially if there is significant harm and legal action seems possible.
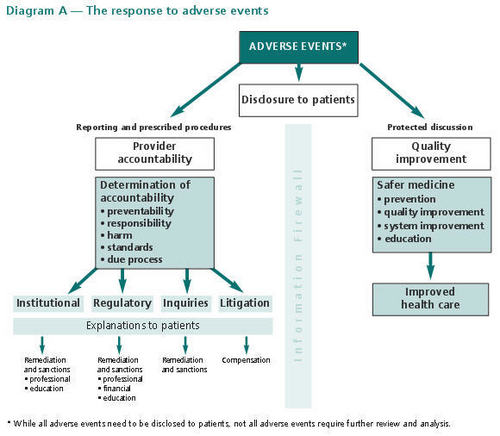
It is clear from this diagram below that disclosure and explanation are not the same thing. Initial disclosure is the communication with the patient that occurs as soon as reasonably possible after an adverse event. This focuses on the known facts and the provision of further clinical care and emotional support. Explanation or post-analysis disclosure is subsequent communication with the patient about known facts related to the harm and reasons for the harm. This occurs after an appropriate analysis of the adverse event. [4]
Why disclose?
Why is it difficult to disclose errors?
The disclosure of harm is a complicated topic and we can not cover it in full detail here, for more information and suggestions please see the CPSO document "Disclosure of Harm"[9] The duty to disclose does not end with disclosure to the patient. It may be necessary to report adverse events within institutions or to other outside organizations.
While it is uncomfortable to disclose our own errors it is even more complicated and uncomfortable to disclose the errors of others.
The CPSO offers some suggestions when commenting on the mistakes of others:
"Inappropriate Words" should not be spoken. Gratuitous negative comments about care provided by other physicians (verbally or in the chart) are never appropriate. Neither should you pass severe judgement or censure colleagues or staff in front of patients, visitors or other staff.
When commenting on the work of a colleague, consider advising the other physician, to disclose your difference of opinion with that physician. It is good practice to clarify the situation and to work toward the responsible physician making the disclosure to the patient.
Consider calling the CMPA for advice.
Responsibilities of the Resident in the event of harm
Report your own mistakes (large or small) to your supervisor. Staff physicians should decide whether, when and how to disclose to the patient and apologize.
The CPSO policy on Postgraduate learners states: A Postgraduate learner who has advised the Most Reponsible Physician and his or her Clinical Preceptor that a patient has sustained harm has fulfilled his or her obligation for disclosure." Your duty is to disclose to your attending.
Whistle blowing and reporting the errors of others
Whistle blowing, or raising awareness within an organization of potential wrong doing, is appropriate when the goal is to protect patients from the serious harm to which ignoring such errors might lead.[10]
When it comes to reporting possible errors of incompetence of others, report this information/ your concerns "up the chain of supervision" until you are satisfied with the response.
Remember "just following orders" is not a full defence in law or morality.
When in doubt, contact the CMPA!
Concepts in Tort Law
CONCEPT | DEFINITION | OUTCOME |
Negligence | failure to do what a ’reasonable physician’ would have done under the circumstance | malpractice |
Error of Judgement | a decision/treatment that in hindsight resulted in harm, but that was ’reasonable at the time’ "An error in judgment has long been distinguished from an act of unskillfulness or carelessness or due to lack of knowledge... the honest and intelligent exercise of judgment has long been recognized as satisfying the professional obligation."[6] | no civil liability |
Breached duty of care | malpractice | civil suit to compensate victim for damages caused by wrongful act (’harm’) |
Apology
Yes, this is a clinical skill for professionalism!
The elements of a medical apology include:
Acknowledgment and explanation of wrong
Expression of regret
Medical plan to address current condition
Assurance that it will not happen to others
it may also include consideration of restitution/compensation and or advise to consult a lawyer
What does the CMPA have to say about apology?[8]
"If harm is the result of an adverse event related to an inherent risk of an investigation or treatment: An expression of regret should be provided, such as "I feel badly that this happened to you." An apology (with acceptance of responsibility) should not be provided."
If harm is the result of an adverse event related to system failures of provider performance, as determined after careful analysis, and apology should be considered by the responsible provider or responsible organization. The use of words that express or imply legal responsibility, such as negligence or fault, or reference to failing to meet the standard of care, should be avoided and are not part of disclosure.
Is an apology and admission of guilt?
There is indeed a medico-legal dilemma with apology. A genuine apology, including taking responsibility and providing assurance that it will not happen again, makes litigation less likely. However, an admission of responsibility makes any litigation that might occur more likely to succeed.
The Apology Act (Ontario 2009) addresses some of these issues and clarifies that an apology is considered to be an expression of sympathy or regret, a statement that a person is sorry or any other words or actions indicating contrition or commiseration, whether or not the words or actions admit fault. An apology does not, in law, constitute an express or implied admission of fault or liability by the person in connection with the matter.

_________________________________
1. Baker GR, Norton PG, Flintoft, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. CMAJ 2004;170(11):678-86.
2. Patient Safety Competencies Framework. Canadian Patient Safety Institute. cited December 7, 2009. Available from: www.patientsafetyinstitute.ca/English/education/safetyCompetencies/Pages/KeyMessages.aspx
3. For more on the role of communication and patient safety please see the Communication for Patient Safety module (not required as part of this module, but supplementary information).
4. Reporting and responding to adverse events: A medical liability perspective. Ottawa, ON: Canadian Medical Protective Association; 2009. www.cmpa-acpm.ca/cmpapd04/docs/submissions_papers/com_reporting_and_responding_to_adverse_events-e.cfm accessed August 2, 2011
5. Disclosure Working Group. Canadian Disclosure Guidelines. Edmonton, AB: Canadian Patient Safety Institute; 2008
6. From Wilson v. Swanson, [1956] S.C.R. 804 (S.C.C.) at 812
7. CMA Code of Ethics (Update 2004) policybase.cma.ca/PolicyPDF/PD04-06.pdf accessed August 2, 2011
8. Apology legislation in Canada: What it means to you. Originally published September 2008. available at: www.cmpa-acpm.ca/cmpapd04/docs/resource_files/infosheets/2008/com_is0889-e.cfm accessed August 2, 2011
9. CPSO: Disclosure of Harm Policy Number: #5-10 Reviewed and Updated: May 2010 www.cpso.on.ca/policies/policies/default.aspx?ID=1578 accessed August 2, 2011
10. Doyle L. Whistle blowing: the ethics of revealing professional incompetence within dentistry. British Dental Journal.1993;174:95-101.
 Previous
Previous


